Scalpels Down, Mouths Open: Doctors Can’t Stop Interrupting Each Other!
In the fast-paced world of healthcare, the operating room is often seen as a bastion of precision, respect, and coordination. However, beneath the sterile lights and synchronized procedures lies an often overlooked challenge: communication breakdowns among medical professionals. While doctors wield scalpels with deftness, they are far less disciplined when it comes to conversations with one another. The phenomenon of frequent interruptions among doctors is a growing concern that affects not only professional relationships but also patient care.
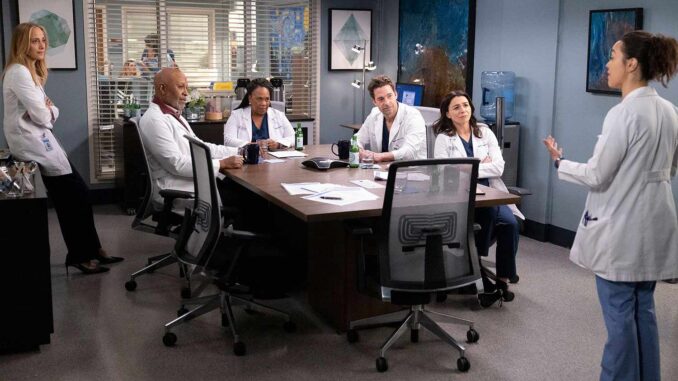
Studies in hospital settings have shown that even among seasoned professionals, communication isn’t always seamless. Discussion among doctors, especially during consultations or interdisciplinary team meetings, is frequently riddled with interruptions, cut-offs, and overlapping dialogue. These interruptions, while sometimes benign or unintentional, can lead to miscommunications and even errors in diagnosis or treatment. In environments where collaboration is key, communication should flow smoothly and respectfully.
Here are a few reasons why interruptions among doctors occur more often than we think:
- Time Pressure: With limited time to assess patients and make decisions, doctors often rush to contribute their points, sometimes inadvertently interrupting others.
- Hierarchical Dynamics: Senior doctors may dominate conversations, consciously or unconsciously sidelining the opinions of younger colleagues.
- Cognitive Overload: In complex cases, eagerness to share an idea or recollection might lead to speaking out of turn.
- Communication Styles: Different personalities and training backgrounds influence how doctors engage in discussions.
However, the impact goes beyond awkward pauses and bruised egos. Inefficient communication can lead to:
- Reduced Team Cohesion: Persistent interruptions can erode trust and collaboration.
- Inaccurate Patient Information: Crucial insights may be missed if a speaker is interrupted before finishing.
- Delayed Decision-Making: Disconnected dialogue can stretch discussions and prolong critical choices.
To counter this, many hospitals are introducing interventions such as communication training programs, emphasizing structured discussions like the SBAR (Situation, Background, Assessment, Recommendation) technique, and reminding teams of the importance of professional respect in all exchanges. Active listening is now being recognized as a skill as vital as surgical precision or diagnostic acumen.
Ultimately, when doctors put their scalpels down, it’s crucial that they open their mouths with mindfulness. Each voice in the room matters—not just for harmonious teamwork but for the lives that hang in the balance. After all, excellent healthcare doesn’t just rely on what is said—but on what is heard.